Clinical Management of Asthma in Primary Care
Click on the tabs below to learn more.
There is no gold standard test to diagnose asthma. The diagnosis of asthma is made based on characteristic history and is supported by positive obstructive airflow variability and reversibility with spirometry. In primary care, besides clinical history, asthma diagnosis has predominantly been made from a trial of medication. Hence, over- and under-diagnosis of asthma are common due to the lack of objective lung function testing to demonstrate variable expiratory airflow limitation.
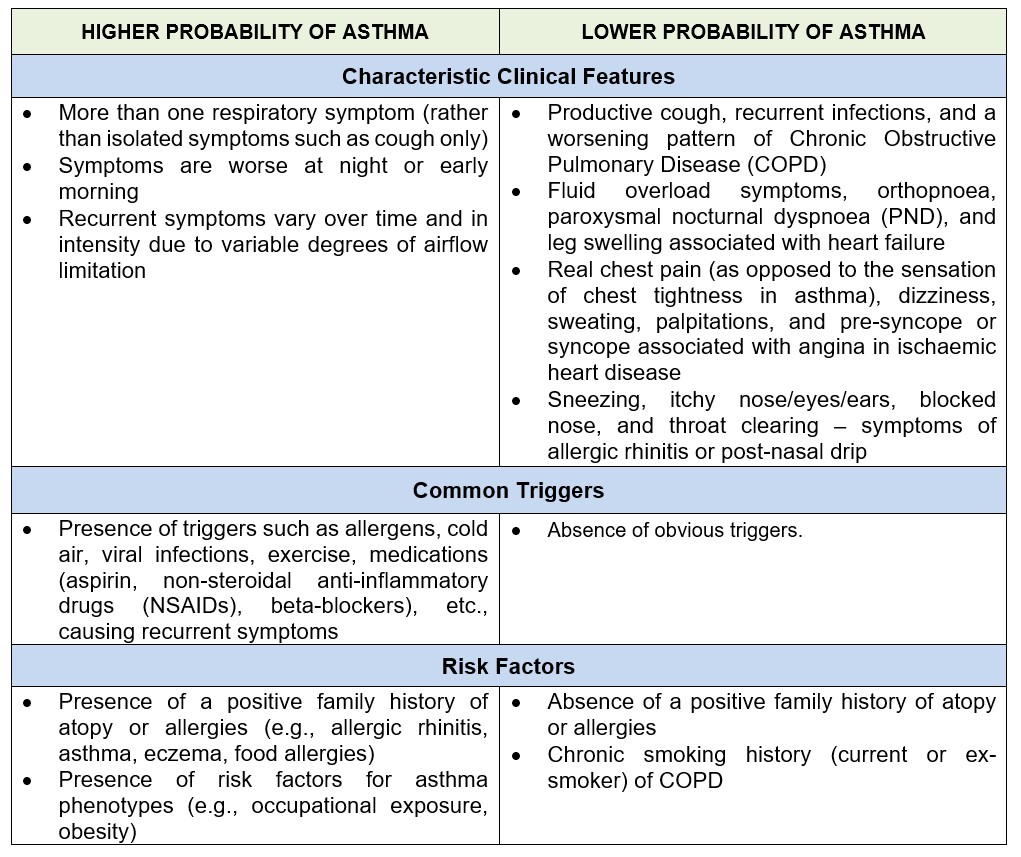
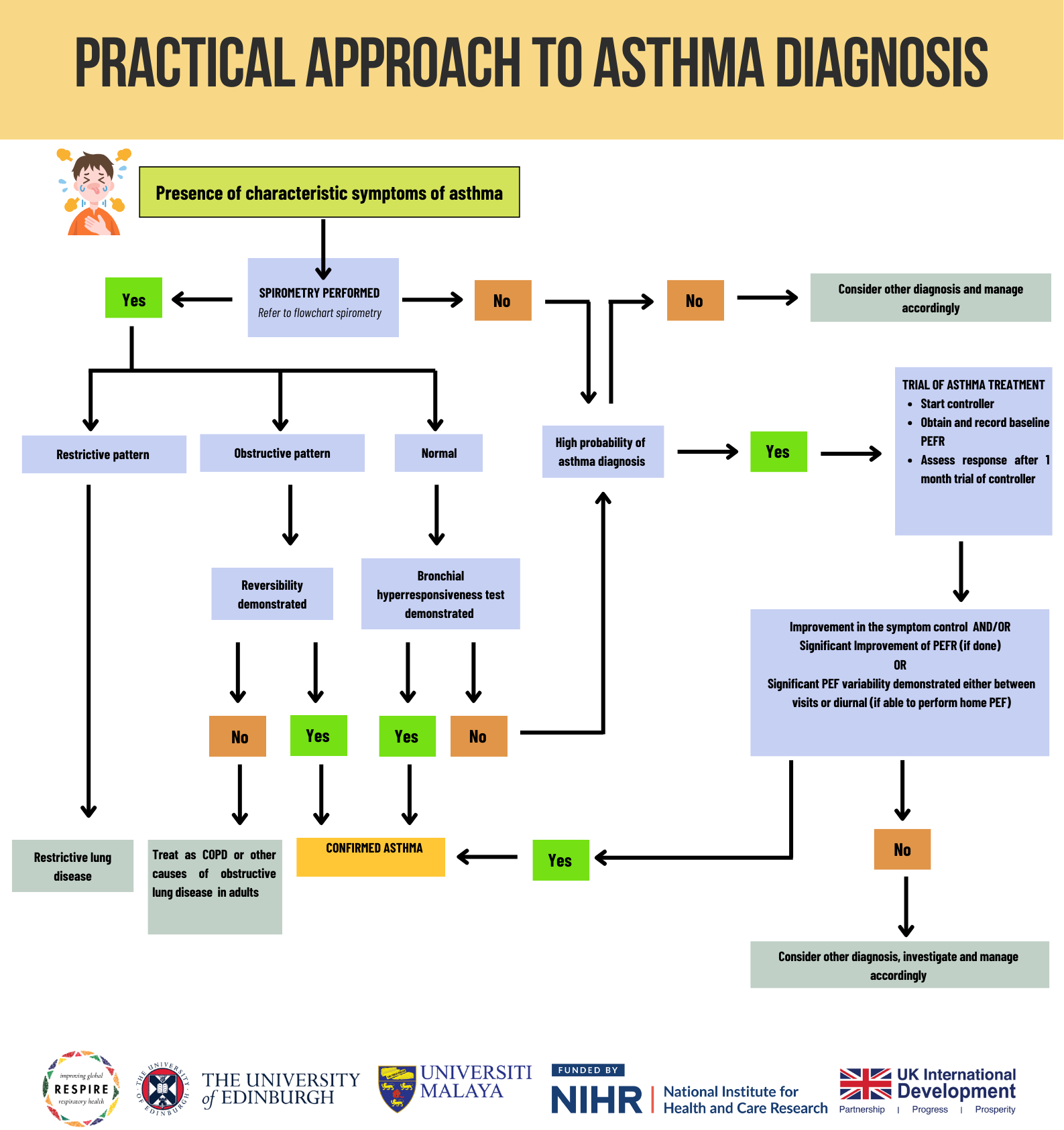
Although spirometry is more reliable for objective measurements of airflow limitation, it is not always available or easily accessible in primary care. Given the resource-limited setting, alternative approaches to diagnosing asthma in primary care are acceptable. Demonstrating excessive airflow variability using peak expiratory flow rate (PEFR) is acceptable with the presence of characteristic symptoms. PEFR is the maximal flow achieved during the maximally forced expiration initiated at full inspiration.
A. Positive bronchodilator reversibility test:
Increase from baseline in PEFR, 10 – 15 minutes after 200 – 400 mcg of salbutamol.
- Adult ≥ 20 %
- Children ≥ 15%
B. Diurnal PEFR variability:
- PEFR each morning and evening over 1 to 2-week period
- Excessive diurnal variability - > 10 % for adults and > 13 % for children
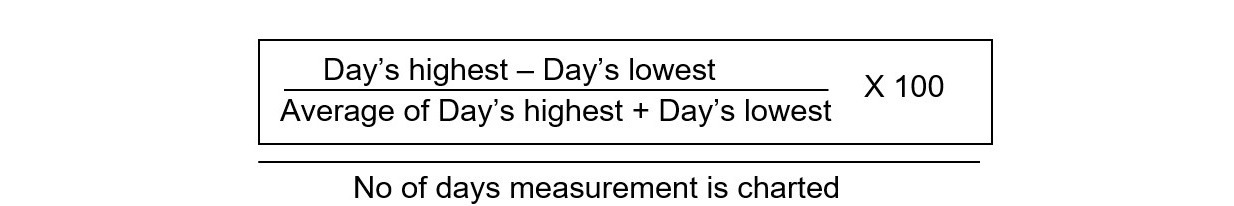
- Example of diurnal variability calculation using daily amplitude percent mean method:
C. Significant improvement of PEFR with anti-inflammatory:
With respiratory symptoms characteristic of asthma, a significant improvement by >20% from the baseline after 4 weeks of anti-inflammatory treatment (such as inhaled corticosteroid).
D. PEFR variation between visits:
With respiratory symptoms characteristic of asthma, a change of PEF of at least >20% for adults and >15% for children between visits is accepted.
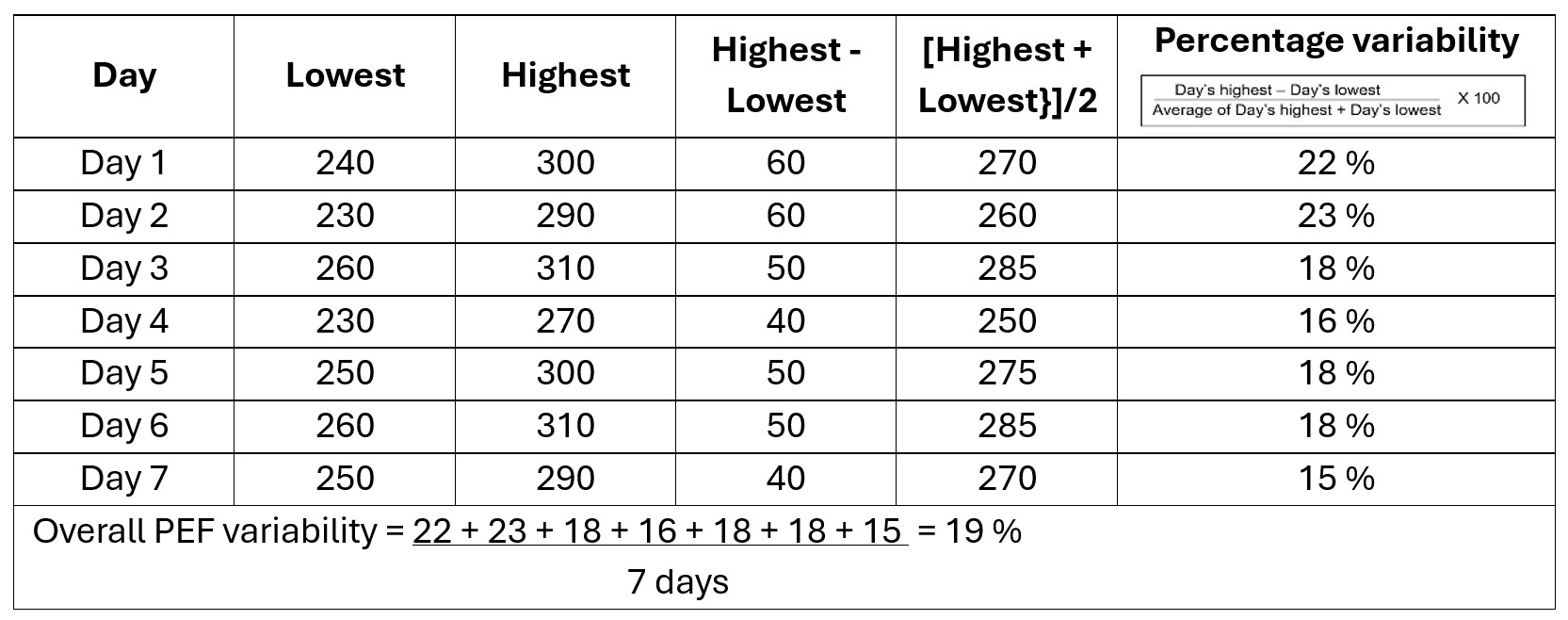
Asthma is a chronic condition that requires ongoing management to ensure symptoms are controlled, quality of life is maintained, and complications are minimised. Regardless of the control level, all patients with asthma should have a regularly scheduled review (follow-up). Individuals with asthma need to adhere to their scheduled appointments for effective monitoring. In an ideal team-based asthma care setting, a comprehensive assessment package could be delivered through collaborative work between team members with appropriate training in asthma, each carrying their own defined roles. A team-based asthma care should include at least doctors, nurses, and pharmacists. However, in a setting with limited human resources and/or a heavy patient load, patients with poorly controlled asthma should be prioritised to receive as comprehensive an assessment and care as possible. Patients with good asthma control should at least receive a basic assessment of care. The routine care for all patients with asthma, performed during each review, should incorporate evidence-based quality indicators. These assessments should also be performed whenever appropriate during the patient’s unscheduled clinic encounters.
Click on the tabs below to learn more.
Pharmacotherapy
Two types of medication are used in the treatment of asthma.
- Reliever medications work quickly and are used to treat acute symptoms.
- Controller medications work slowly over time and are taken regularly to prevent asthma attacks.
Asthma pharmacotherapy is based on two classes of drugs:
- Anti-inflammatory
- Work by suppressing the inflammation that narrows the airways.
- Must be taken regularly (every day) and continuously.
- Inhaled corticosteroid (ICS) and ICS-long-acting beta2 agonist (LABA) combinations have been the mainstay maintenance therapies for asthma.
- Inhaled corticosteroids
- Oral corticosteroids (OCS)
- Leukotriene receptor antagonists
- Monoclonal antibodies
- Bronchodilators Reliever medications that help to relax and dilate (widen) the narrowed airways resulting in asthma symptoms.
- Short-acting β-agonist (SABA)
- Long-acting beta-agonist (LABA)
- Anti-inflammatory relievers (AIR)
- Anti-inflammatory drugs are used as anti-inflammatory relievers (AIR) because they relieve symptoms while reducing inflammation (used as needed).
- AIR drugs include ICS-formoterol (Symbicort®).
- Antimuscarinic
Initiating Pharmacotherapy
12 years and older
The GINA strategy divides the treatment recommendations for patients 12 years and older into two tracks.
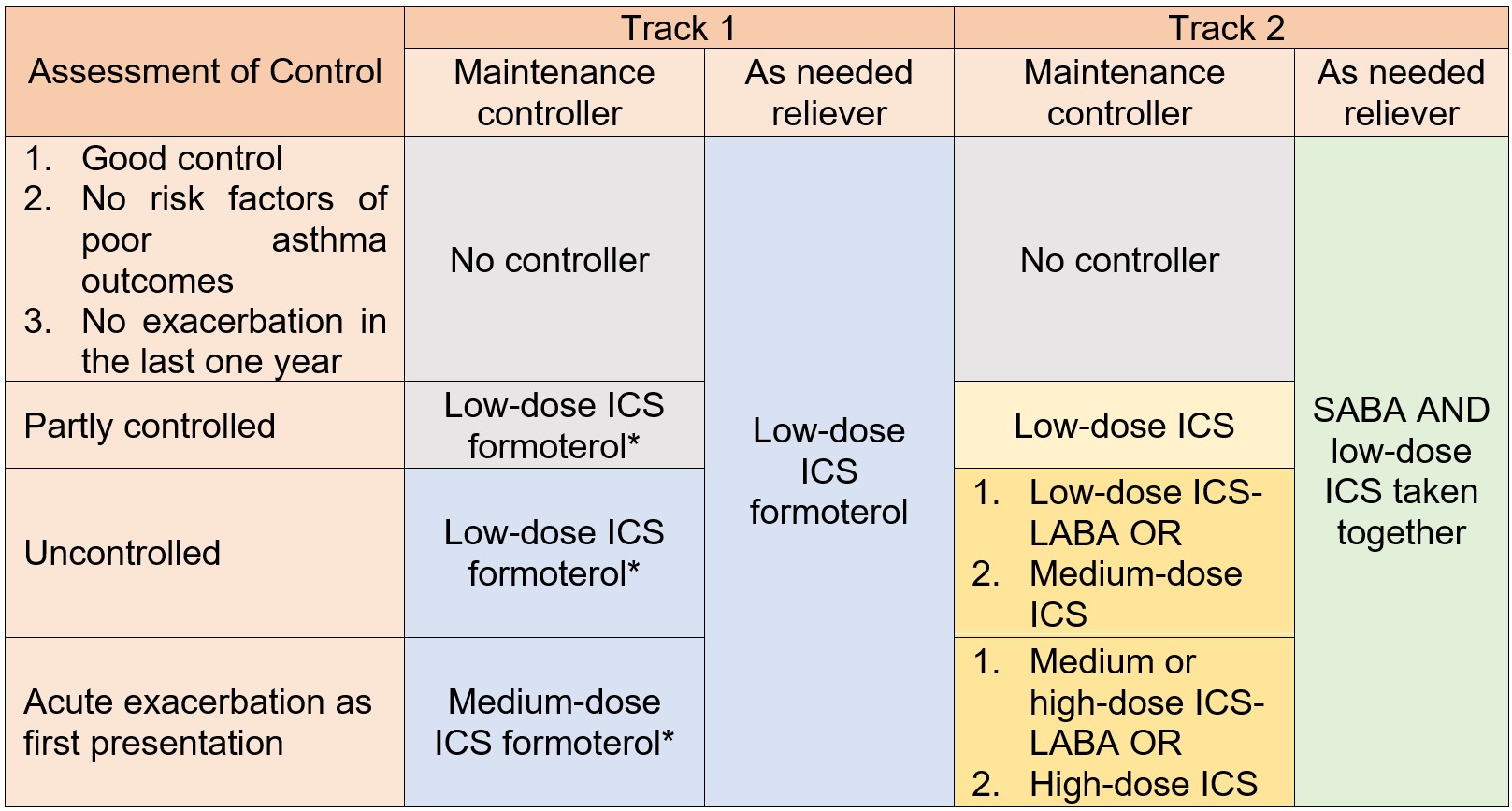
* MART (maintenance and reliever therapy)
- Track 1
- use as-needed combination low-dose ICS-formoterol as the reliever
- simpler
- Track 2
- use as needed SABA as the reliever along with a separate preventer inhaler
6 – 11 years
The GINA strategy divides the treatment recommendations of patients 6 to 11 years as below.
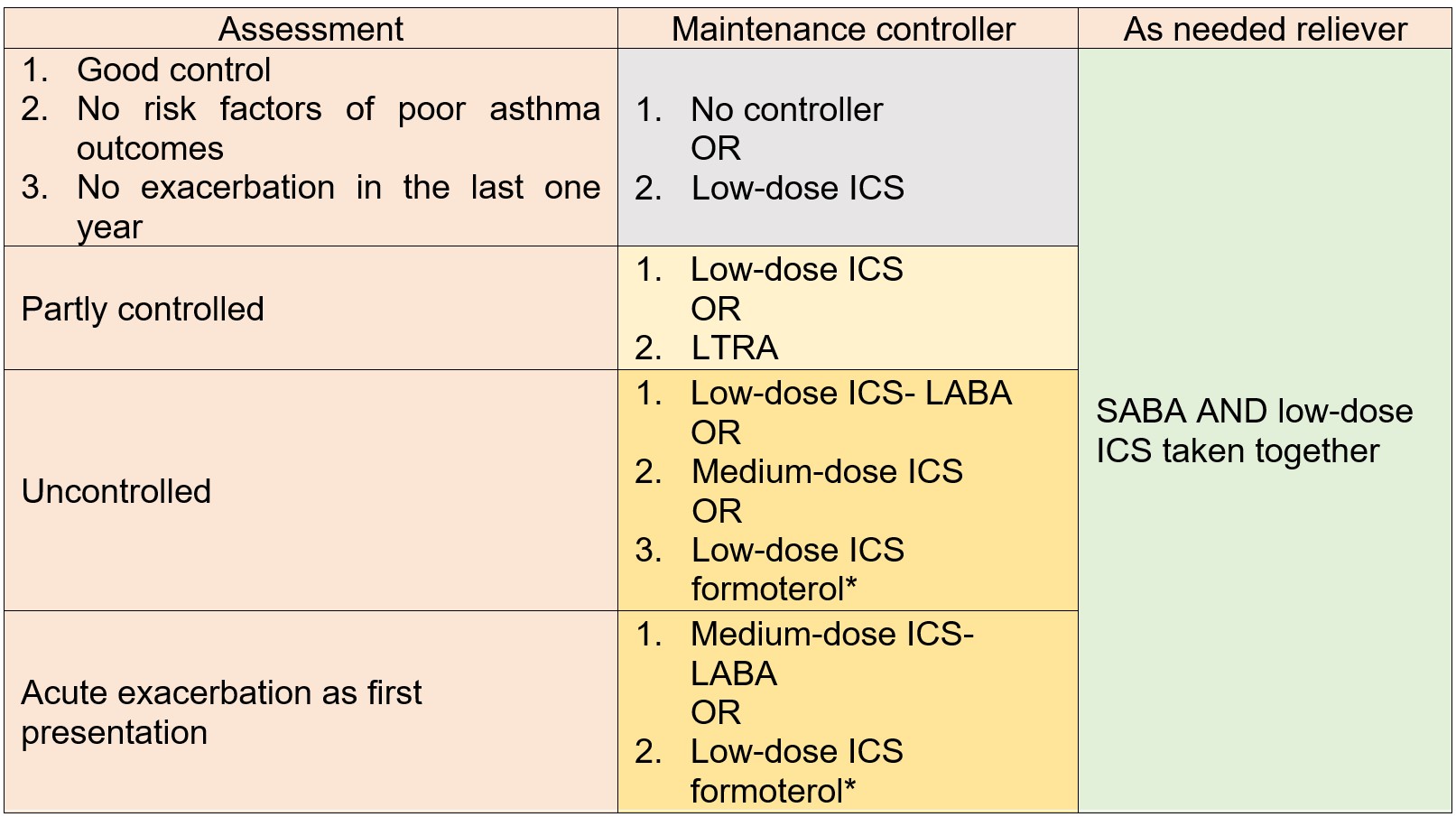
* MART (maintenance and reliever therapy)
Optimising Pharmacotherapy
Appropriate adjustment to the treatment regimen may be necessary and should be considered in certain situations such as:
- Poor symptoms control
- Frequent exacerbations
- Adherence issue
- Inability to use the inhaler device correctly
- Pregnancy in adult patients
Treatment optimisation can be guided by the GINA 2024 recommendation by step-up and step-down strategies towards the right and the left of the ladder respectively.
Stepping Up the Pharmacotherapy
- Short-term step-up (1 to 2 weeks)
- Worsening symptoms (e.g. during viral infection)
- According to the Asthma Action Plan (yellow zone)
- Sustained step-up (at least 2 - 3 months)
- Worsening symptoms are due to asthma
- Inhaler technique is correct
- Adherence is good
- Modifiable risk factors have been avoided
- Assess response after 2 - 3 months
- Good response: maintain
- No response: step up the GINA treatment ladder
- A patient who fails to achieve good asthma control after appropriate treatment optimisation should be referred to respiratory physicians for further evaluation and/or pharmacotherapy intensification.
Consider stepping up the treatment for patients with poor asthma control when all the following aspects have been checked:
Stepping Down the Pharmacotherapy
Consider stepping down asthma treatment when a patient:
- Has achieved good control of asthma for at least 3 months
- Has no history of exacerbations in the last year
- Does not have any current medical condition potentially worsening asthma control (e.g. chest infection, travelling, or pregnancy)
- Checklist for the pharmacotherapy step-down process
- Patient is informed, explained, and agrees
- Asthma action plan is reinforced
- The step-down is done gradually, at intervals of at least 3 months
- Regular follow-up is provided for close monitoring
Non-pharmacotherapy
Asthma management is not just about drug treatment. Non-pharmacological interventions are an important aspect and should be used in combination with medications. If pharmacotherapies are not sufficient to achieve good asthma control, confounding factors such as poor treatment adherence, poor inhaler technique, comorbidities, and exposure to modifiable risk factors should first be ruled out before increasing therapy dosage or resorting to add-on treatments.
The patient's active participation is important in asthma management. All patients should be made aware of the components of asthma self-management, which include:
- Self-monitoring of symptoms and/or PEF
- An asthma action plan for optimisation of asthma control through self-adjustment of medications
- A regular medical review by healthcare providers
Refer to the Targeted Asthma Education section for more detail.
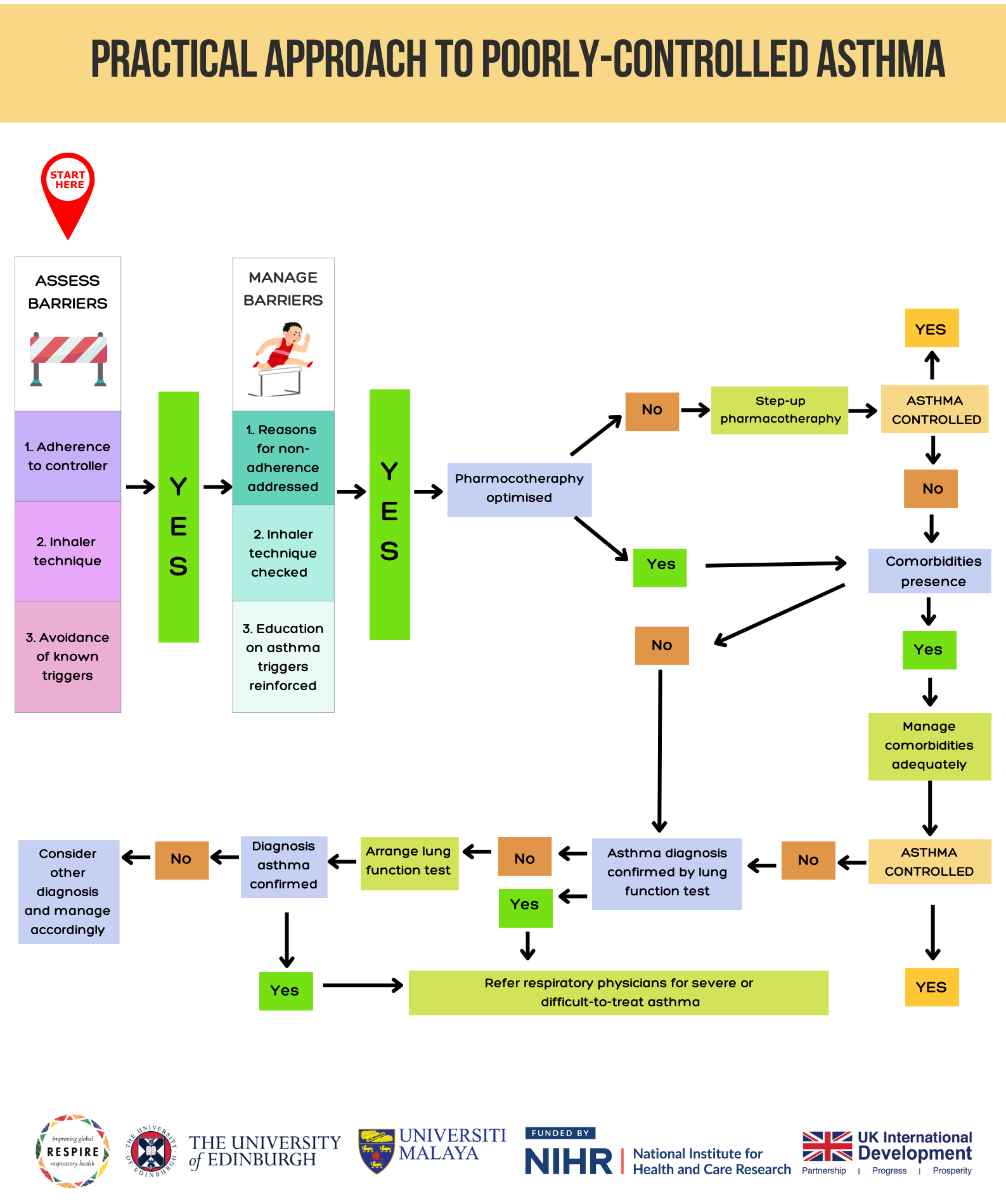
A practical approach to managing poorly controlled asthma involves a systematic evaluation to identify and address underlying issues. Initially, it is crucial to assess and confirm the patient's inhaler technique and adherence to the prescribed treatment regimen. Incorrect use of inhalers and poor adherence are common causes of suboptimal asthma control.
Additionally, identifying and mitigating modifiable risk factors, such as exposure to allergens, tobacco smoke, or environmental pollutants, is essential. Regularly reviewing and updating the patient's asthma action plan can help ensure they are following the appropriate steps during exacerbations. If asthma control remains poor despite these measures, consider stepping up pharmacotherapy according to the Global Initiative for Asthma (GINA) guidelines.
In cases where asthma control is still not achieved, a referral to a specialist for further evaluation and potential treatment adjustment may be necessary. This structured approach helps in pinpointing and resolving factors contributing to poor asthma control, thereby improving patient outcomes.
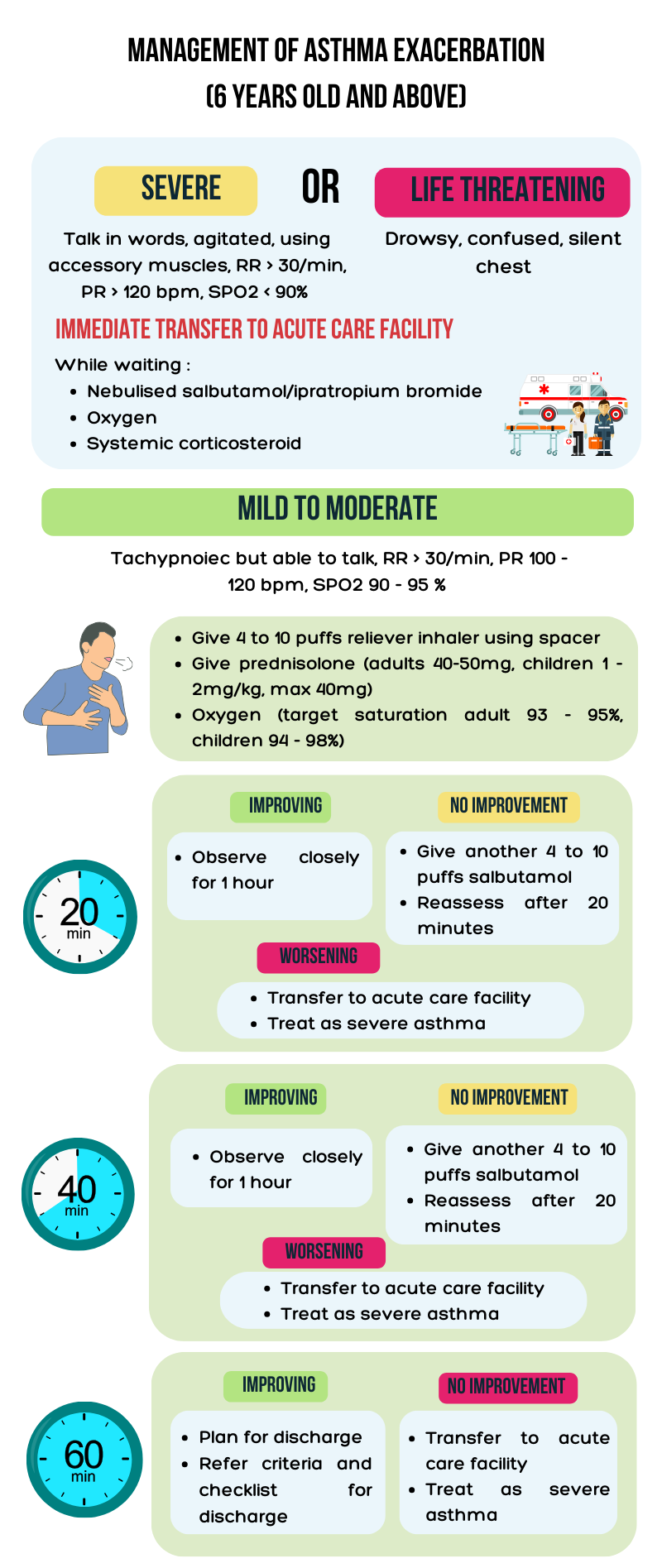
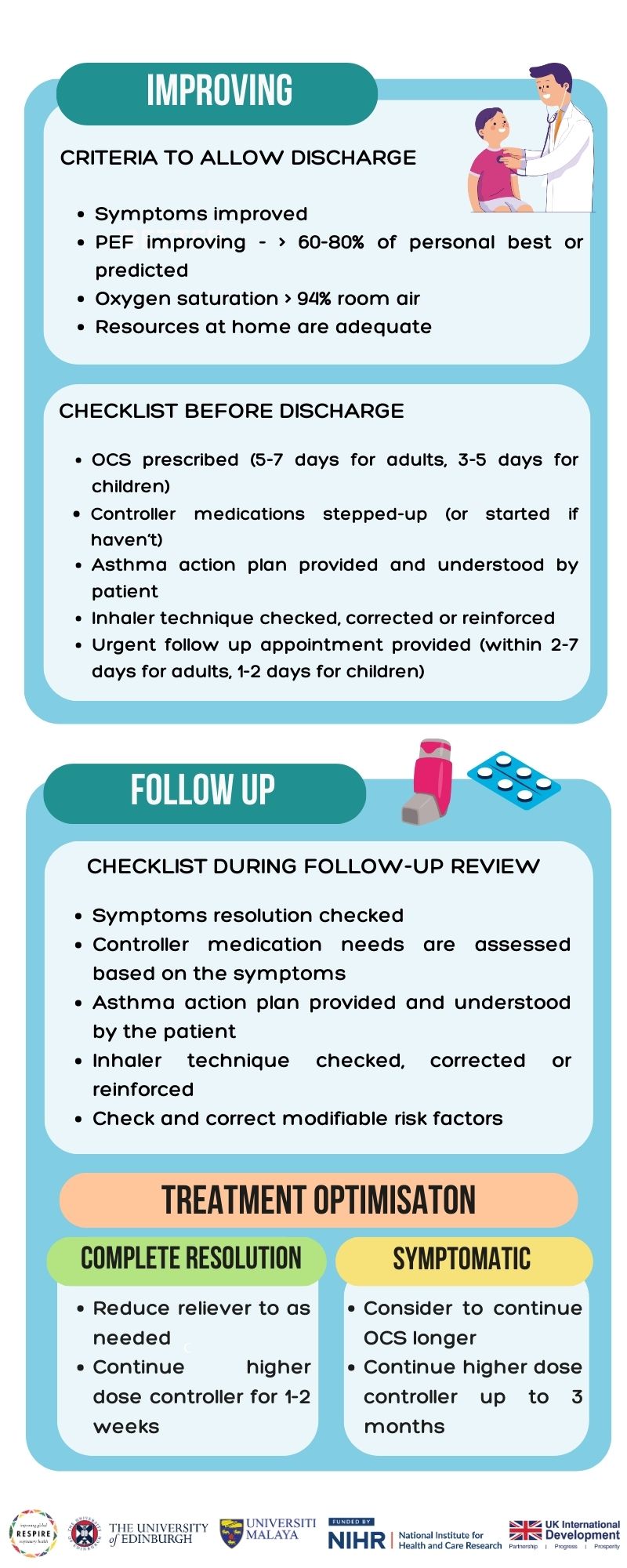
Asthma exacerbation is a progressive decrease in lung function characterised by a progressive increase in symptoms of SOB, cough, wheezing or chest tightness. Asthma exacerbation treatment aims to relieve symptoms and return patients to their best lung function. For most patients, initial treatment with nebulised β-agonist and oral corticosteroids is sufficient. Supplemental oxygen is indicated for hypoxaemia and should be given at a flow rate or concentration sufficient to maintain oxygen saturation > 90%. Hospitalisation is generally required if the patient's condition worsens or fails to improve after optimal treatment for exacerbation has been provided.