Targeted Asthma Education
Asthma education is a fundamental aspect of asthma management. Effective asthma education empowers patients to take control of their asthma and lead healthy, active lives while minimising the risk of exacerbations and complications. Asthma education should be tailored to meet the individual needs and preferences of patients and caregivers, considering factors such as age, language, cultural background, health literacy, and socioeconomic status.
Asthma education should include the important components below (click to see the details):
Asthma is a chronic condition that affects the airways in our lungs. Imagine your airways as tiny tubes carrying air in and out smoothly. In asthma, these airways become inflamed and narrowed, making it harder to breathe. Exposure to various triggers can irritate the airways, causing inflammation. This process subsequently narrows the air passages and leads to the symptoms of asthma.
The classic symptoms of asthma are:
- Shortness of breath or a feeling of tightness in the chest
- Coughing, especially at night or early in the morning
- Wheezing, which is a whistling sound when breathing
Although many people develop asthma during childhood, it is not uncommon for it to start for the first time at various stages of adulthood. There are many different types of asthma, each with its own features and characteristics. These are known as asthma phenotypes.
Some well-recognised asthma phenotypes include:
- Allergic asthma
- Non-allergic asthma
- Occupational asthma
- Asthma triggered by certain medications, such as aspirin and NSAIDs
Achieving good asthma control is crucial. When asthma is well-managed, a patient will have a good quality of life. They will experience no symptoms during the day or night, have unlimited physical activities including daily living, exercise, and play, and will not miss school or work. Poorly controlled asthma causes frequent symptoms and necessitates the use of a reliever inhaler, emergency room visits, or hospital admission due to exacerbations, which can lead to life-threatening and fatal outcomes. If asthma control remains poor in the long term, lung function will be significantly compromised and permanently reduced.
A patient’s understanding of ‘control’ may not align with the clinical assessment of healthcare professionals. Hence, there is often a mismatch between the professional assessment of control and patients’ perceptions. Patients with poorly controlled asthma may consider their asthma to be ‘well-controlled’, not regard it as serious, and accept their symptoms as part of the ‘norm’ of having asthma. As a result, they may under-report their symptoms, leading to the risk of receiving inadequate treatment.
Identifying and avoiding asthma triggers is essential for minimising symptoms and preventing exacerbations. Education should include information about common triggers and strategies for reducing exposure to them.

Asthma and Obesity
Obesity is a significant risk factor for asthma, and the prevalence of asthma is higher among individuals with obesity compared to those with normal weight. Asthma in individuals with obesity may be more difficult to control with standard treatments compared to non-obese individuals. This may be due to factors such as reduced responsiveness to inhaled corticosteroids, poorer lung function, and increased airway inflammation. Obesity-related comorbidities such as gastroesophageal reflux disease (GERD), obstructive sleep apnoea (OSA), and metabolic syndrome are more prevalent in individuals with both asthma and obesity.
Asthma and Comorbidities
Asthma is usually associated with pulmonary and extrapulmonary comorbidities. Gastroesophageal reflux disease, allergic rhinitis, obesity, depression, diabetes mellitus, and cardiovascular disease are commonly associated comorbidities. Comorbidities in asthma may contribute to poor asthma symptom control by aggravating or mimicking asthma symptoms. This, in turn, may lead to misdiagnosis and overtreatment with anti-asthma medication.
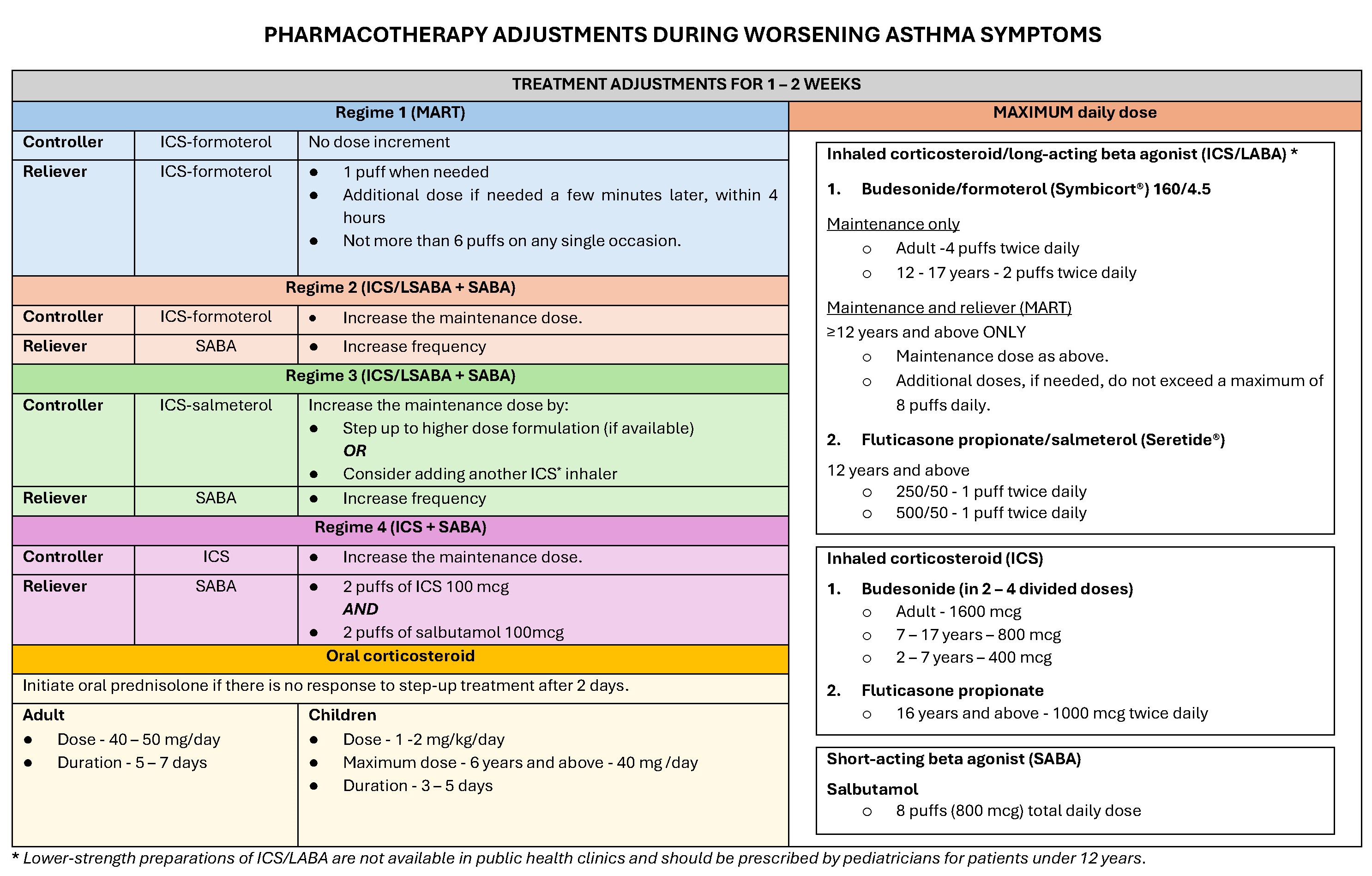
Essentially, there are two types of asthma medications: relievers and controllers. Refer to the section on 'Clinical Management of Asthma' for more information about asthma pharmacotherapy.
Importance of Controller Medications
Controller medications are the cornerstone of asthma treatment. However, many patients may consider these medications unnecessary and may not take them regularly. This can result in uncontrolled asthma and a poor quality of life.
There are several reasons why patients do not take their controller medications:
- Unsure of the indication to take controller medication (inhaler) regularly.
- Concerns About Side Effects: Patients may worry about the long-term side effects of corticosteroids. They should rest assured that since the medication is taken via inhaler, it goes directly to their lungs, minimising the amount that reaches other parts of their body.
- Harmful Effects of Reliever Medication Overuse: Many people with asthma rely too heavily on their reliever inhalers. Using reliever inhalers too often indicates that their asthma is not well-controlled. Patients are at increased risk of frequent and severe exacerbations, and even asthma-related death, if they use three or more canisters of reliever inhalers per year.
Satisfactory technique of inhaler use must be checked and ensured, especially among patients with inadequate control of asthma. The inhaler technique is crucial for the effective management of asthma. Patients' inhaler technique should be checked, corrected if necessary, and reinforced periodically, especially among those with poorly controlled asthma. Watch the videos below to learn more.
7 steps to using a dry powder inhaler
(2 min 10 sec)
7 steps to using a metered dose inhaler
(1 min 6 sec)
7 steps to using a metered dose inhaler and large spacer - front view (1 min 14 sec)
7 steps to using a metered dose inhaler and large spacer - side view (1 min 19 sec)
7 steps to using a metered dose inhaler and medium spacer - front view (1 min 15 sec)
7 steps to using a metered dose inhaler and medium spacer - side view (1 min 15 sec)
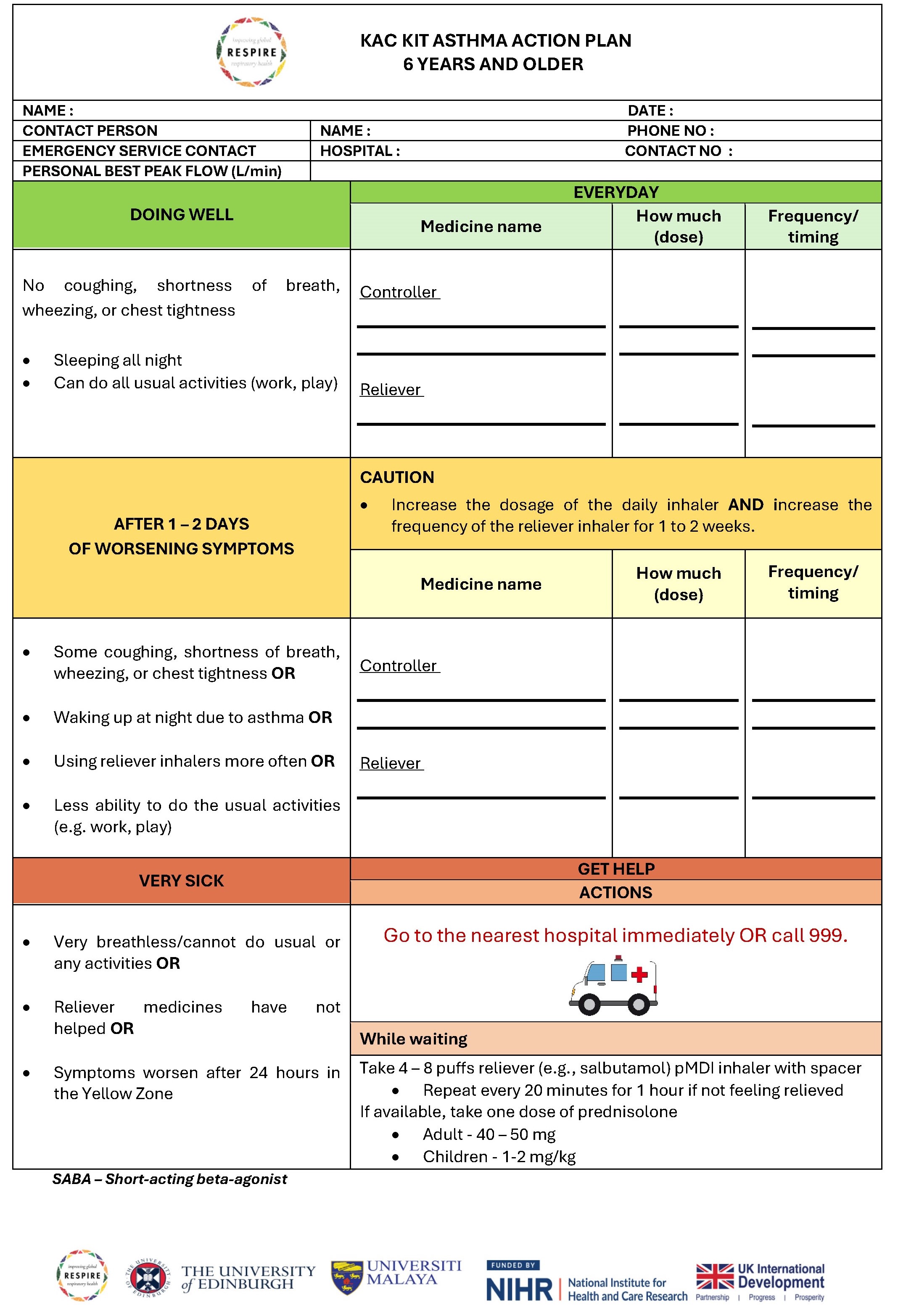
RESPIRE KAC-Kit Asthma Action Plan
Every patient with asthma should have a personalised asthma action plan. An asthma action plan is a written or pictorial document that guides patients in self-managing their asthma effectively. The AAP should outline the steps for daily asthma management, including medication use, symptom monitoring, recognition of symptom changes, and actions to take in response to worsening symptoms or exacerbations.